Multiple Myeloma - Overcoming the Challenges
Nov. 22, 2023 #Multiple Myeloma
Introduction
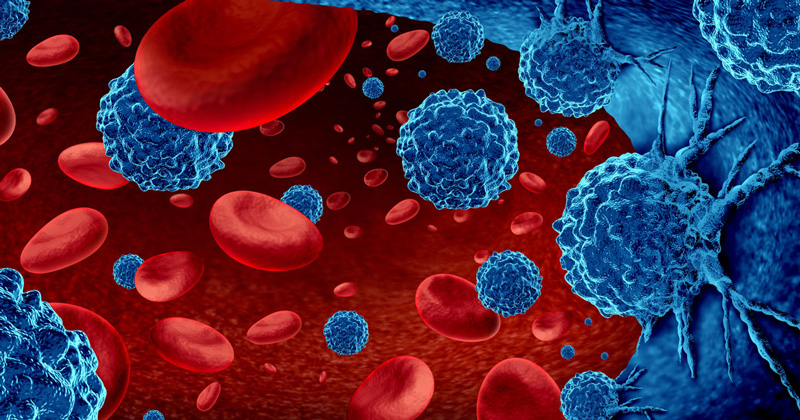
Multiple myeloma is a complex and often challenging blood cancer that affects plasma cells, a type of white blood cell responsible for producing antibodies. This condition disrupts the normal balance of blood cell production and can lead to a range of symptoms.
In this comprehensive guide, we will define multiple myeloma, explore its causes and symptoms, discuss the diagnostic process, and elucidate the various treatment options available to manage this hematologic malignancy.
Defining Multiple Myeloma
Multiple myeloma, often referred to simply as myeloma, is a cancer of plasma cells—specialized white blood cells found in the bone marrow. Plasma cells play a crucial role in the immune system by producing antibodies that help the body fight infections. In multiple myeloma, these plasma cells become cancerous and multiply uncontrollably, crowding out normal blood-forming cells in the bone marrow.
The accumulation of malignant plasma cells can lead to the production of abnormal proteins, which can cause a variety of complications, including bone damage, anemia, and impaired immune function. Multiple myeloma is considered a hematologic malignancy, falling under the umbrella of cancers affecting the blood and bone marrow.
Causes of Multiple Myeloma
The exact cause of multiple myeloma remains unclear, but certain risk factors and genetic abnormalities have been identified. Key factors associated with an increased risk of developing multiple myeloma include:
Age:
Multiple myeloma is more commonly diagnosed in older adults, with the majority of cases occurring in individuals over the age of 65. The risk increases with age.
Gender:
Men are slightly more likely to develop multiple myeloma than women.
Race and Ethnicity:
African Americans are at a higher risk of developing multiple myeloma compared to individuals of other racial or ethnic backgrounds.
Family History:
Having a first-degree relative (parent, sibling or child) with multiple myeloma or a related plasma cell disorder may increase the risk.
Monoclonal Gammopathy of Undetermined Significance (MGUS):
MGUS is a condition in which abnormal plasma cells are present in the bone marrow, but the levels of abnormal proteins are lower than those seen in multiple myeloma. MGUS is considered a precursor to multiple myeloma, and individuals with MGUS have an increased risk of progression to myeloma over time.
Genetic Factors:
Certain genetic mutations and chromosomal abnormalities have been associated with an increased risk of multiple myeloma. These genetic factors can contribute to the uncontrolled growth of plasma cells.
While these risk factors may increase the likelihood of developing multiple myeloma, the majority of individuals diagnosed with the condition do not have an identifiable cause. Ongoing research aims to unravel the complex interplay of genetic and environmental factors contributing to the development of multiple myeloma.
Symptoms of Multiple Myeloma
The symptoms of multiple myeloma can vary widely, and some individuals may not experience noticeable symptoms in the early stages of the disease. Common symptoms include:
Bone Pain:
Persistent bone pain, often in the back, hips or ribs, is a common symptom of multiple myeloma. The cancerous plasma cells can accumulate in the bone marrow, leading to bone damage and pain.
Fatigue and Anemia:
Anemia is a condition characterized by a decrease in red blood cells which can result in fatigue and weakness.
Increased Susceptibility to Infections:
The compromised immune function associated with multiple myeloma can lead to an increased susceptibility to infections.
Kidney Problems:
The abnormal proteins produced by cancerous plasma cells can impair kidney function, leading to symptoms such as increased thirst, frequent urination, and swelling.
Unexplained Weight Loss:
Unintentional weight loss may occur as a result of the metabolic changes associated with multiple myeloma.
Frequent Bruising and Bleeding:
Impaired blood clotting due to a decrease in platelets can result in easy bruising and bleeding.
Nausea and Constipation:
The accumulation of abnormal proteins can affect the digestive system, leading to symptoms such as nausea and constipation.
Neurological Symptoms:
In rare cases, multiple myeloma may cause neurological symptoms, such as weakness, numbness or tingling, due to compression of nerves by cancerous plasma cells.
It's important to note that these symptoms can be indicative of various conditions, and a thorough medical evaluation is necessary for an accurate diagnosis.
Diagnosis of Multiple Myeloma
The diagnosis of multiple myeloma involves a combination of clinical assessments, laboratory tests, and imaging studies. Key components of the diagnostic process include:
Blood and Urine Tests:
Complete Blood Count (CBC): A CBC measures the levels of red blood cells, white blood cells, and platelets. Anemia and other blood abnormalities may be indicative of multiple myeloma.
Blood Chemistry Panel: This panel assesses the levels of various substances in the blood, including calcium, creatinine and albumin. Abnormalities may suggest kidney dysfunction or other complications.
Urine Protein Electrophoresis: This test helps identify abnormal proteins (M-proteins) in the urine, a common feature of multiple myeloma.
Bone Marrow Aspiration and Biopsy:
A bone marrow aspiration and biopsy involve collecting a sample of bone marrow from the hipbone or another large bone. The sample is examined under a microscope to assess the presence of cancerous plasma cells and determine the extent of involvement.
Imaging Studies:
X-rays: X-rays may be performed to detect bone abnormalities, such as fractures or lesions.
Computed Tomography (CT) Scan: CT scans provide detailed images of the bones and other tissues, helping to evaluate the extent of bone damage.
Magnetic Resonance Imaging (MRI): MRI scans may be used to assess bone marrow involvement and detect lesions in soft tissues.
Positron Emission Tomography (PET) Scan: PET scans can help identify areas of increased metabolic activity, providing information about the extent and location of the disease.
Genetic and Chromosomal Testing:
Testing for specific genetic mutations and chromosomal abnormalities associated with multiple myeloma can provide valuable information about the prognosis and potential treatment options.
Staging:
Multiple myeloma is staged based on the extent of involvement and the presence of specific symptoms. Staging helps guide treatment decisions and predict the course of the disease.
The comprehensive evaluation of clinical, laboratory and imaging findings is crucial for confirming a diagnosis of multiple myeloma and determining the most appropriate treatment approach.
Treatment Options for Multiple Myeloma
The management of multiple myeloma is complex and often involves a combination of therapies tailored to the individual's specific circumstances. Treatment goals include controlling the disease, alleviating symptoms and improving overall quality of life. Common treatment modalities include:
Chemotherapy:
Chemotherapy involves the use of drugs to kill or control cancer cells. Various chemotherapy regimens may be employed, and the choice of drugs depends on factors such as disease stage and patient health.
Immunomodulatory Drugs (IMiDs):
Drugs such as thalidomide, lenalidomide and pomalidomide are classified as immunomodulatory drugs and have demonstrated effectiveness in treating multiple myeloma. They work by modulating the immune system and inhibiting the growth of cancerous plasma cells.
Proteasome Inhibitors:
Medications like bortezomib, carfilzomib and ixazomib are proteasome inhibitors that interfere with the normal functioning of cells, including cancer cells. They help prevent the breakdown of proteins and promote the destruction of cancerous plasma cells.
Stem Cell Transplantation:
Autologous stem cell transplantation involves harvesting a patient's own stem cells, administering high-dose chemotherapy to eliminate cancer cells, and then reinfusing the harvested stem cells to restore blood cell production. Allogeneic stem cell transplantation, which uses stem cells from a donor, is less commonly performed.
Monoclonal Antibodies:
Monoclonal antibodies, such as daratumumab, elotuzumab and isatuximab, target specific proteins on the surface of cancerous plasma cells, enhancing the immune system's ability to recognize and destroy these cells.
Corticosteroids:
Corticosteroids, such as dexamethasone or prednisone, may be included in treatment regimens to reduce inflammation and suppress the activity of abnormal plasma cells.
Radiation Therapy:
Localized radiation therapy may be used to target specific areas of bone affected by myeloma, providing relief from pain and helping to control disease progression.
Targeted Therapies:
Emerging targeted therapies, such as selinexor and venetoclax, aim to specifically target pathways involved in the growth and survival of cancer cells, offering additional treatment options.
Supportive Care:
Supportive care measures, including medications for pain management, treatment of anemia, and prevention of infections, are essential components of multiple myeloma care.
Precautions and Considerations
Regular Monitoring:
Individuals undergoing treatment for multiple myeloma require regular monitoring of blood counts, kidney function, and other parameters to assess treatment response and detect any potential complications.
Management of Side Effects:
Treatment for multiple myeloma may be associated with side effects, such as fatigue, nausea, and increased susceptibility to infections. Effective management of these side effects is crucial for optimizing the individual's quality of life.
Supportive Services:
Access to supportive services, including counseling, nutritional support and palliative care, can enhance the overall well-being of individuals with multiple myeloma and their caregivers.
Participation in Clinical Trials:
Participation in clinical trials may be considered as part of the treatment plan, providing access to innovative therapies and contributing to advancements in the field.
Genetic Counseling:
Individuals with multiple myeloma and their families may benefit from genetic counseling to understand the implications of specific genetic mutations and assess the risk of familial predisposition.
Collaboration with Healthcare Team:
Open communication and collaboration with a multidisciplinary healthcare team, including hematologists, oncologists, nurses and supportive care professionals, are essential for comprehensive and individualized care.
Conclusion
Multiple myeloma presents complex challenges, requiring a nuanced and multidimensional approach to diagnosis and treatment. Advances in our understanding of the genetic and molecular mechanisms driving the disease have paved the way for targeted therapies and personalized treatment strategies.
While multiple myeloma remains an incurable condition, ongoing research and innovation continue to expand treatment options and improve outcomes for individuals affected by this hematologic malignancy. The collaborative efforts of healthcare professionals, researchers and individuals with multiple myeloma contribute to a collective journey toward more effective treatments and, ultimately, a brighter outlook for those facing this challenging blood cancer.








COMMENTS