Lipoedema - Understanding Body Fat
Nov. 21, 2023 #Diabetes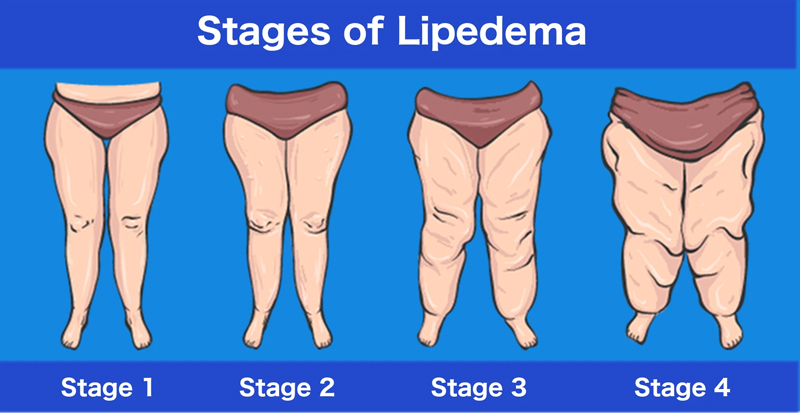
Introduction
Lipoedema, often spelled as lipedema, is a chronic condition characterized by the abnormal and disproportionate accumulation of fat, primarily in the legs and buttocks. This condition predominantly affects women and is often underdiagnosed, leading to challenges in managing its physical and emotional impact.
In this comprehensive guide, we will define lipoedema, explore its potential causes, delve into the symptoms that distinguish it, and discuss various treatment options available to individuals coping with this unique and often misunderstood condition.
Defining Lipoedema
Lipoedema is a chronic adipose tissue disorder characterized by the abnormal and symmetrical accumulation of fat, typically in the lower body, especially the hips, thighs and lower legs. Unlike general obesity, lipoedema results in a disproportional distribution of fat, creating a distinct "column-like" appearance. The affected areas often present with a nodular or lobular texture due to the accumulation of excess fat.
Causes of Lipoedema
The exact cause of lipoedema remains unclear, and the condition is believed to have a multifactorial origin involving genetic, hormonal and environmental factors. Key considerations regarding the potential causes of lipoedema include:
Genetic Predisposition:
Lipoedema often appears to have a familial or genetic component. Individuals with a family history of lipoedema are at an increased risk of developing the condition. Specific genetic factors contributing to lipoedema are an area of ongoing research.
Hormonal Influences:
Hormonal changes, particularly those associated with puberty, pregnancy, and menopause, may play a role in the development or exacerbation of lipoedema. The condition is most commonly diagnosed in women and hormonal fluctuations are believed to contribute to the abnormal accumulation of fat.
Vascular and Lymphatic Factors:
Lipoedema is often associated with vascular and lymphatic dysfunction. Impaired blood flow and lymphatic drainage may contribute to fluid retention and the deposition of fat in affected areas.
Inflammatory Factors:
Inflammation is thought to play a role in the development of lipoedema. Chronic low-grade inflammation may contribute to the expansion of fat cells and the characteristic changes in adipose tissue seen in lipoedema.
Pregnancy and Hormonal Changes:
The hormonal changes associated with pregnancy can influence the severity of lipoedema symptoms. Many women report the onset or worsening of lipoedema during or after pregnancy.
Environmental Triggers:
While genetic and hormonal factors are significant, environmental factors such as a sedentary lifestyle, poor diet, or trauma may exacerbate lipoedema symptoms. Lifestyle modifications can influence the progression and management of the condition.
Symptoms of Lipoedema
Lipoedema presents with characteristic signs and symptoms that distinguish it from general obesity or other fat distribution disorders. Recognizing these symptoms is crucial for accurate diagnosis and appropriate management. Key symptoms of lipoedema include:
Bilateral and Symmetrical Fat Accumulation:
Lipoedema typically affects both legs symmetrically, creating a characteristic column-like appearance. The fat accumulation is often confined to the hips, thighs, and lower legs, sparing the feet.
Nodular or Lobular Texture:
The affected areas may exhibit a nodular or lobular texture due to the presence of enlarged fat cells. This can be felt under the skin and may contribute to tenderness or discomfort.
Pain and Tenderness:
Individuals with lipoedema may experience pain or tenderness in the affected areas, especially during activities or pressure on the tissue. The pain is often described as aching or throbbing.
Easy Bruising:
The skin in lipoedema-affected areas is often fragile, and individuals may experience easy bruising or the formation of small blood vessels near the skin's surface (telangiectasias).
Orthostatic Edema:
Lipoedema-related edema tends to worsen with prolonged standing or sitting and improves with elevation or rest. This orthostatic component distinguishes it from other conditions with localized fat accumulation.
No Involvement of Feet:
Unlike conditions such as lymphedema, lipoedema typically spares the feet. The feet maintain a relatively normal appearance, creating a distinct demarcation at the ankles.
Progressive Nature:
Lipoedema is often progressive, with symptoms worsening over time. The condition may initially be mistaken for simple weight gain, but the distinct pattern and disproportionate distribution of fat characterize lipoedema.
It's important to note that individuals with lipoedema may have a normal body mass index (BMI) or be only mildly overweight, emphasizing the distinction between lipoedema and general obesity.
Treatment Options for Lipoedema
The management of lipoedema involves a multidisciplinary approach aimed at reducing symptoms, improving quality of life and addressing associated complications. While there is no cure for lipoedema, various treatment options can help manage the condition effectively. Key treatment modalities for lipoedema include:
Conservative Measures:
Compression Therapy: Wearing compression garments, such as compression stockings or leggings, can help reduce edema and provide support to the affected tissues. Graduated compression garments are often recommended to promote lymphatic drainage.
Manual Lymphatic Drainage (MLD): MLD, performed by trained therapists, involves gentle massage techniques to stimulate lymphatic flow and reduce fluid retention. MLD is often used in conjunction with compression therapy.
Decongestive Exercises: Engaging in low-impact exercises, such as swimming or walking, can promote circulation and help manage lipoedema symptoms. Exercises should be tailored to individual capabilities and avoid excessive strain on the affected areas.
Nutritional and Lifestyle Modifications:
Healthy Diet: Adopting a balanced and nutritious diet can contribute to overall health and weight management. Nutritional counseling may be beneficial to address specific dietary needs and promote weight loss if applicable.
Regular Exercise: Incorporating regular, low-impact exercise into the routine can support overall health and contribute to weight management. Exercises that promote flexibility and circulation are particularly beneficial.
Medical Therapies:
Pain Management: Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to manage pain and discomfort associated with lipoedema.
Liposuction: In cases where conservative measures are insufficient, liposuction may be considered to remove excess fat deposits. Water-assisted liposuction (WAL) and tumescent liposuction are among the techniques used for lipoedema. Liposuction can provide long-term improvement in symptoms but may not be a cure.
Psychological Support:
Counseling and Support Groups: Given the emotional impact of lipoedema, counseling and participation in support groups can help individuals cope with the challenges of living with a chronic condition. Addressing body image concerns and fostering a positive mindset are integral aspects of holistic care.
Surgical Interventions:
Excisional Surgery: In cases of severe lipoedema with excess skin or fibrous tissue, excisional surgery may be considered. This involves removing excess tissue to improve the overall contour of the affected areas.
Therapeutic Lymph Node Transfer: This surgical procedure involves transferring healthy lymph nodes to the affected areas to enhance lymphatic drainage.
Hormonal and Medicinal Approaches:
Hormonal Therapies: Some practitioners explore hormonal therapies, such as hormonal contraceptives, to manage lipoedema symptoms. However, research on the effectiveness of hormonal interventions is limited, and individual responses may vary.
Precautions and Considerations
Individualized Treatment Plans:
Lipoedema is a highly individualized condition, and treatment plans should be tailored to each person's specific symptoms, preferences and overall health. Collaborative decision-making with healthcare providers is crucial.
Long-Term Management:
Lipoedema requires ongoing management and a commitment to lifestyle modifications for long-term success. Regular follow-up with healthcare providers ensures that treatment plans are adjusted as needed.
Monitoring for Complications:
Individuals with lipoedema should be monitored for potential complications, including infections, cellulitis, and changes in skin integrity. Prompt attention to any signs of infection is essential.
Psychological Well-Being:
Addressing the psychological impact of lipoedema is integral to comprehensive care. Mental health support, counseling and participation in support groups can contribute to a positive mindset and improved overall well-being.
Educational Resources:
Accessing reliable educational resources and staying informed about lipoedema can empower individuals to actively participate in their care. Knowledge about the condition, available treatments and lifestyle strategies is essential.
Conclusion
Lipoedema poses unique challenges due to its distinct pattern of fat accumulation and the potential impact on physical and emotional well-being. While there is no cure for lipoedema, a combination of conservative measures, medical therapies and surgical interventions can effectively manage symptoms and improve quality of life.
By fostering a collaborative relationship with healthcare providers, embracing a holistic approach to care, and prioritizing lifestyle modifications, individuals with lipoedema can navigate the complexities of their condition and work towards optimal management. Ongoing research and awareness initiatives contribute to advancing our understanding of lipoedema, paving the way for improved treatment options and support for those affected by this often overlooked disorder.












COMMENTS